Unveiling the Complexities of Medical Malpractice Statistics
Delving into the intricate realm of medical malpractice, a recent analysis spanning the years 1991 to 2005 offers a revealing glimpse into the landscape of malpractice claims across 25 medical specialties in the United States. This study ventures beyond mere statistics, delving into the nuanced interplay between physicians' specialties, age demographics, and the multifaceted repercussions of malpractice litigation.
Diving into the heart of the matter, the study shines a spotlight on the cumulative risk faced by physicians practicing in high and low-risk specialties. Picture this: a cohort of physicians spanning the ages of 30 to 70, navigating the labyrinth of their careers amidst the looming specter of malpractice claims.
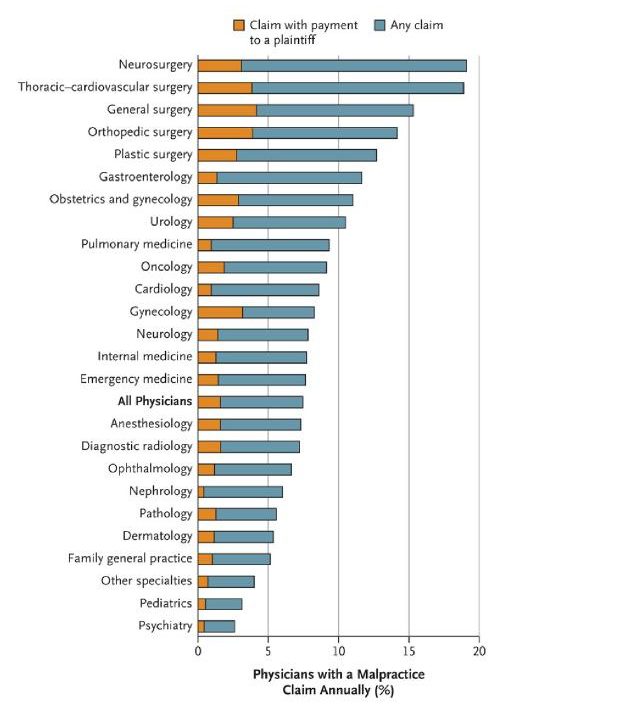
Here's where the numbers start to tell a tale of their own. With an average malpractice claim rate of 7.4% per year, and a mere 1.6% of claims resulting in payments to plaintiffs, the precarious tightrope of litigation looms large over the medical profession. Surprisingly, a staggering 78% of claims end without any financial settlement, leaving physicians to grapple with the fallout of unfounded accusations.
Where do these insights come from, you might ask? The data, sourced from a nationwide insurance society covering over 40,000 physicians and spanning 233,738 physician-years of coverage, paints a vivid portrait of malpractice trends across all 50 states. Notably, the Golden State of California emerges as an outlier, overrepresented with a malpractice claim rate of 12.2%.
Now, let's talk specialties. Brace yourself for a rollercoaster ride of risk assessment. From the adrenaline-charged realms of neurosurgery and thoracic-cardiovascular surgery to the meticulous domains of pathology and dermatology, the spectrum of risk varies wildly. High-risk specialties like orthopedic surgery and obstetrics-gynecology boast claim rates upwards of 10%, while their low-risk counterparts hover around the 5% mark.
But here's the kicker: the real game-changer lies in the age-old adage of time. By the age of 65, a staggering 99% of physicians in high-risk specialties will have faced at least one malpractice claim, compared to a relatively modest 75% in low-risk fields. By age 45, a third of high-risk specialists have already weathered the storm of litigation, compared to a mere 5% in low-risk specialties.
Beyond the raw numbers lies a labyrinth of factors shaping physicians' perceptions of malpractice. From the looming shadow of potential claims to the mental and emotional toll of litigation, the ramifications extend far beyond mere financial settlements. Interestingly, nearly 40% of claims are untethered to medical errors, highlighting the broader implications of defensive medicine and its impact on patient care.
In conclusion, the study paints a sobering picture of the pervasive nature of medical malpractice in high-risk specialties, underscoring the intense pressure to practice defensive medicine. Yet, amidst the sea of litigation, evidence suggests that the scope of defensive practices remains modest at best, begging the question of whether the ends truly justify the means.
Shifting gears, the study's juxtaposition with the landscape of military healthcare offers a stark reminder of the divergent paths of malpractice litigation. Despite the undeniable commitment to quality care, military physicians operate under a unique set of circumstances, shielded by the controversial Feres doctrine from the legal repercussions of medical errors. While service members are entitled to compensation for service-connected injuries, the opacity surrounding disability evaluation systems leaves much to be desired, with fewer than 40% of wounded military members satisfied with the current process.
In a world where transparency is paramount, the study serves as a clarion call for greater accountability and awareness within the realms of medical malpractice. By shedding light on the multifaceted impacts of litigation and fostering a culture of learning and improvement, we can strive towards a future where patient care reigns supreme, unencumbered by the shadows of litigation and opacity.
Anupam B. Jena, Seth Seabury, Darius Lakdawalla, Amitabh Chandra – Malpractice risk according to physician specialty, N. Engl. J. Med 2011;365: 629-636
Sandeep S Mangalmurti, Lindsey Murtagh, Michelle M. Mello – Medical malpractice in the military - N. Engl. J. Med 2011; 365: 664-670
Specialties of Focus for Wired Raven NPM
Oral Surgery
Neurosurgery
Anesthesiology
Opthomology
Dermatology
Dentistry
Pediatrics
Dentistry
Orthopedics
Plastic Surgery
OBGYN
Urology
Dermatology
